Case Study: Recouped Rebates
Fortune 500 Company Recoups $1M during Rebate Reconciliation


Case Study: Recouped Rebates
Fortune 500 Company Recoups $1M during Rebate Reconciliation
Client Profile
Members Covered: 144,000+ | Prescriptions Filled Annually: 1.2M | Savings: $1M
Members Covered: 144,000+
Prescriptions Filled Annually: 1.2M
Savings: $1M
The Challenge
After the Fortune 500 company hired Remedy Analytics to help manage its Rx benefits, Remedy performed its annual financial savings report (FSR). When comparing it to the rebate reporting from the client’s PBM, Remedy discovered a huge disparity. The rebate claim counts and resulting payments made to the client did not match what Remedy expected the payments to be. The FSR revealed a difference of 6,000 claims and some $1M in rebates.
The Solution
In light of the significant amount of rebate dollars not paid out to the client, Remedy initiated a Rebate Reconciliation. After a full review of Remedy contract parameters and multiple confirmations with the PBM of what claims should be included versus excluded from the rebate guarantees, there was still a large variance. Remedy continued to scrutinize drug definitions and types to see if the discrepancy was there but could not determine why the disparity was so great.
Next, the pharmacy advocate verified if the Zero Balance Due claims were included in the rebate guarantee, to which the PBM confirmed that they were. Through the review process and with a persistent commitment to discover the reason behind the inconsistency, Remedy determined that the discrepancy matched with the Zero Balance Due claim count. Despite the fact that the PBM confirmed in writing multiple times that Zero Balance Due claims were included in the rebate guarantee per the contract and paid to the client, this was not the case. The PBM finally realized it had made a significant error and had actually excluded Zero Balance Due claims.
“I appreciated the immediate audit Remedy did. Under the typical consultant arrangement, we would have had to wait at least a year for a rebate audit, and I’m quite sure we would not have had a similar result.”
- VP of Benefits
The Results
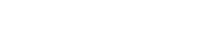
Remedy’s discovery resulted in an additional $1M being paid to the company. In the final analysis, Remedy not only negotiated a favorable contract for the client, but it also was relentless in making sure that the contract was adhered to with its rebate reconciliation.
Remedy Analytics adopted improved process efficiencies in the case and the client gained significant trust with its pharmacy advocate, knowing that Remedy would work tirelessly on its behalf to get the savings it was owed.
Top Benefits Achieved for Client
- Contract protection and data integrity verification enforced to the fullest extent for maximum client reimbursement.
- PharmaLogic® discovered 6,000 claims that had mistakenly been excluded due to the PBM data logic discrepancy.
- Remedy saved the client’s time, money and resources that would have been spent managing a full rebate audit.