PharmaLogic®
Unrivaled visibility into your Rx plan with our revolutionary technology
PharmaLogic® is a game-changer in the prescription drug space

Building PharmaLogic®
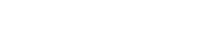
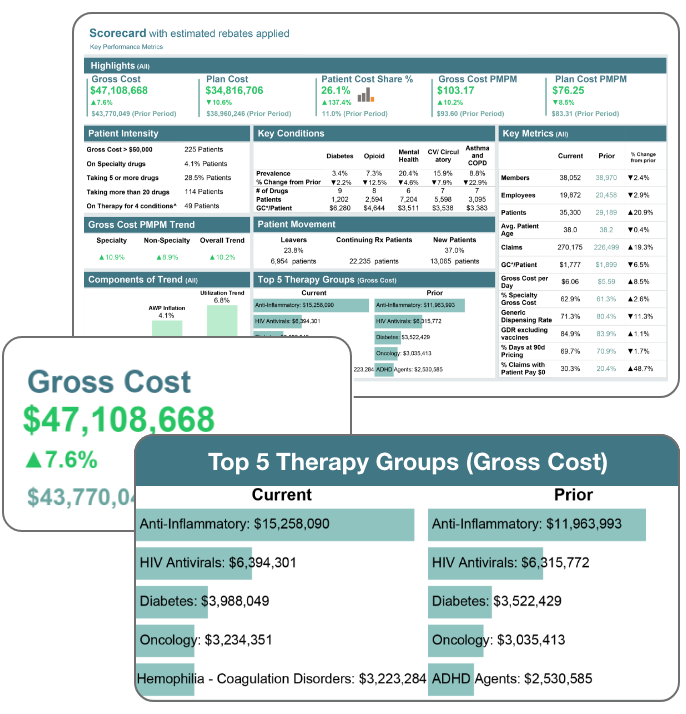
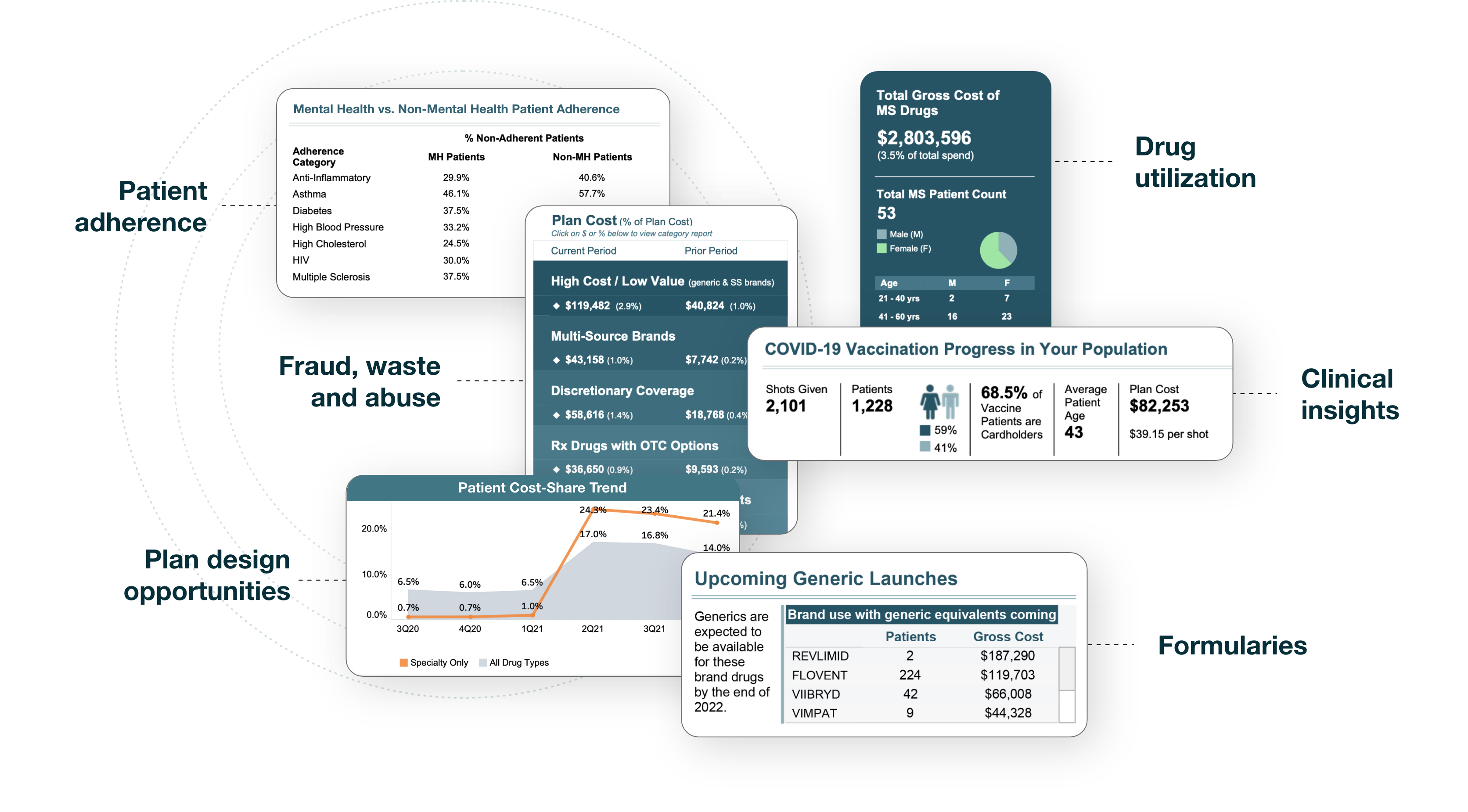
In 2012, Remedy set out to solve a problem: self-insured payers could not see their own Rx claims information, let alone make any sense out of it. Since then, Remedy has invested millions to develop PharmaLogic®, a one-of-a-kind platform that now has more than 60 “Actionboards” and has amassed millions of claims and billions of distinct data points.
The powerful combination of customized interfaces and big data — as well as the Remedy team behind it — leads to optimal management of your Rx plan.
In 2012, Remedy set out to solve a problem: self-insured payers could not see their own Rx claims information, let alone make any sense out of it. Since then, Remedy has invested millions to develop PharmaLogic®, a one-of-a-kind platform that now has more than 60 “Actionboards” and has amassed millions of claims and billions of distinct data points.

The powerful combination of customized interfaces and big data — as well as the Remedy team behind it — leads to optimal management of your Rx plan.
Faster, more informed decision-making
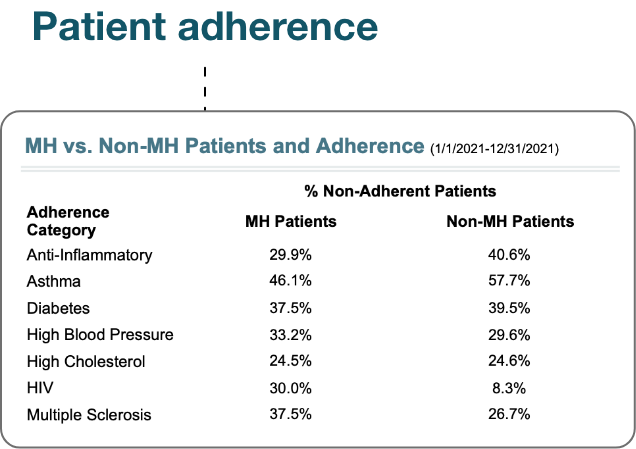
Working with Remedy means you’ll get frequent monitoring throughout the year of claims and access to your own PharmaLogic® portal, so you can make data-backed decisions in real-time.
Reduction in Rx spend
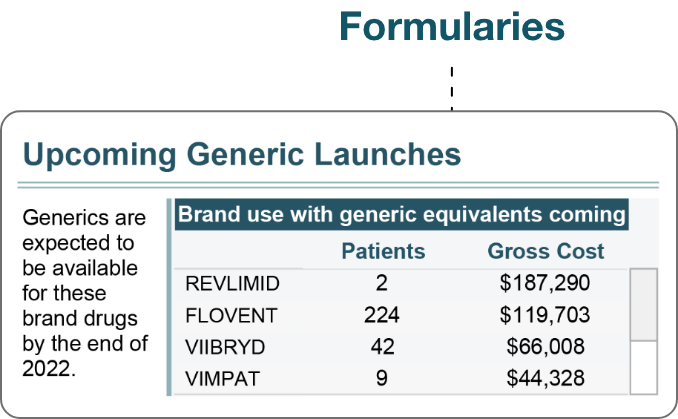
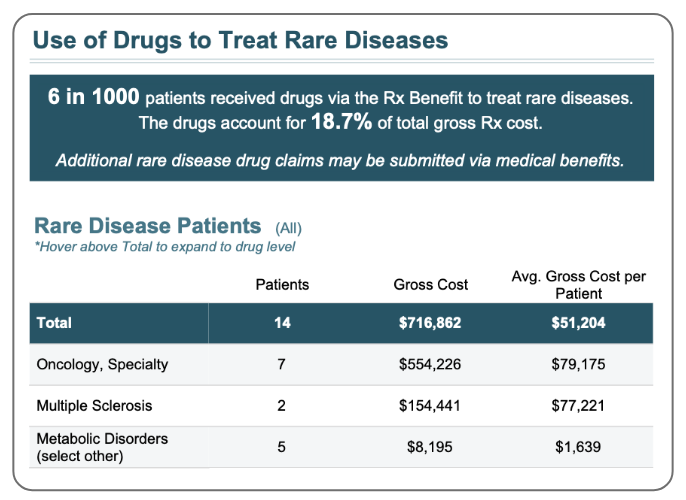
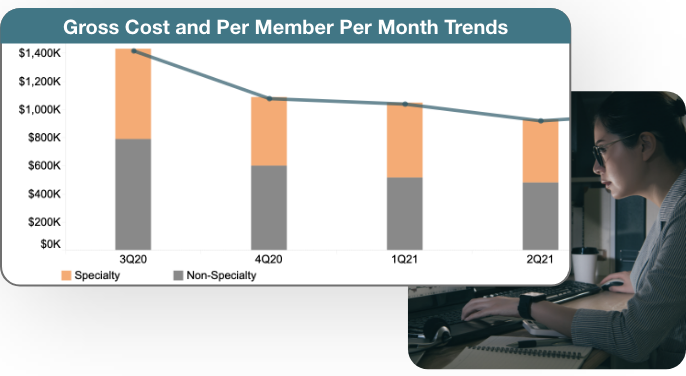
Prescription drug spending has skyrocketed in recent years with no signs of slowing down. PharmaLogic® can help you get a handle on your Rx spend and identify opportunities that can help you meet your specific needs.
Improved forecasting
Staying ahead of the curve prevents surprises in plan performance and allows for you to more effectively budget for the future and proactively consider benefit changes.
Faster, more informed decision-making
Working with Remedy means you’ll get frequent monitoring throughout the year of claims and access to your own PharmaLogic® portal, so you can make data-backed decisions in real-time.
Reduction in Rx spend
Prescription drug spending has skyrocketed in recent years with no signs of slowing down. PharmaLogic® can help you get a handle on your Rx spend and identify opportunities that can help you meet your specific needs.
Improved forecasting
Staying ahead of the curve prevents surprises in plan performance and allows for you to more effectively budget for the future and proactively consider benefit changes.
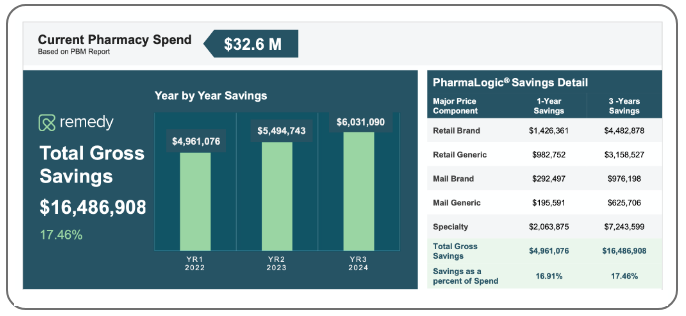
The proof is in the data
Contact us today to see what PharmaLogic® and our actuarial team can uncover.